Specialization






G.I. Cancer Treatments
About Me
Renowned Gastrointestinal Surgeon and Oncosurgeon in Kolkata with extensive experience in GI Oncosurgery, Advanced laparoscopic surgery, piles surgery and management of Complex Digestive Diseases. Comprehensive care of Gastroenterology problems & Comprehensive treatment of all GI cancers. His efficiency in minimally invasive surgery has made him the best laparoscopic surgeon and best Gastrointestinal oncosurgeon in Kolkata…


About Me
Renowned Gastrointestinal Surgeon and Oncosurgeon in Kolkata with extensive experience in GI Oncosurgery, Advanced laparoscopic surgery, piles surgery and management of Complex Digestive Diseases. Comprehensive care of Gastroenterology problems & Comprehensive treatment of all GI cancers. His efficiency in minimally invasive surgery has made him the best laparoscopic surgeon and best Gastrointestinal oncosurgeon in Kolkata…
Why Choose Dr. Sanjoy Mandal-Best Surgical Oncologist in Kolkata
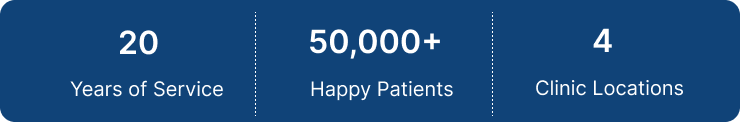
With an experience spanning over 20 years, Dr. Sanjoy Mandal has skillfully performed over 10,000 successful surgeries, benefiting a diverse patient base of over 20,000 individuals. As a leading surgical oncologist in Kolkata, he has expertise in the field of GI Oncosurgery, Advanced laparoscopic surgery, piles treatment and management of complex digestive diseases. Dr. Mandal’s proven track record in minimally invasive techniques, extensive tenure, and compassionate approach collectively make him the best choice for those seeking top-tier gastrointestinal care.




Book your Consultation
Schedule an appointment with Dr. Sanjoy Mandal for personalized and expert care.


Book your Consultation
Schedule an appointment with Dr. Sanjoy Mandal for personalized and expert care.